26 Jun 2025

In the United States, chronic diseases are on the rise, presenting significant challenges for patients, healthcare providers and payers alike. Now more than ever, it's critical for population health executives and quality improvement teams to leverage data and build targeted outreach programs to enhance chronic care management.
The acceleration of chronic conditions in America
In 1995, 118 million people in the U.S. had at least one chronic disease. Today, an estimated 129 million currently live with a chronic disease, and by 2050, the number is projected to rise to 170 million Americans.
Some chronic diseases are especially costly, with chronic kidney disease (CKD), diabetes and hyperlipidemia (cholesterol above 200 mg/dL) being among the most prevalent and costly conditions affecting the population. They not only diminish patients’ quality of life, but also place a significant burden on healthcare systems and resources. Consider:
Targeted interventions that drive lifestyle changes and other preventative measures can improve health outcomes and lower healthcare costs for patients, providers and payers down the road.. The first step in this journey is acquiring impactful data.
Accessing data to identify high- and rising-risk patients
To effectively combat chronic conditions, organizations must identify high- and rising-risk patients. This is where the power of data comes into play.
By leveraging comprehensive laboratory data, electronic health records and claims data, you can gain valuable insights into patient populations. Advanced analytical tools can then process this data to identify patterns and risk factors associated with chronic conditions.
For example, analyzing trends in glucose levels, kidney function markers and lipid profiles can help pinpoint patients at risk of developing or exacerbating chronic conditions.
Data provides actionable insights for targeted interventions
Leveraging data in this manner results in a set of actionable insights that can drive meaningful improvements in patient care. Once the appropriate patients are identified, the next step is to use this information effectively.
Here are four ways you can leverage data for targeted interventions:
- Resource allocation. With data-driven strategies, you can optimize your resources to focus on patients who need interventions the most. Care coordinators receive actionable lists to target patients with overdue testing and identify high- and rising-risk patients, including those with co-morbidities and worsening conditions
- Proactive outreach. Using data to identify patients at risk of deteriorating health, you can engage with them proactively, potentially preventing complications and reducing the need for more intensive interventions down the line
- Personalized care plans. By analyzing each patient's specific risk factors and health status, you can create tailored strategies addressing their individual needs. Developing individualized care plans and personalized engagement strategies ensures patients receive the most appropriate and effective care for their unique situations
- Treatment adherence. You can use data to monitor and improve medication adherence and lifestyle modifications, crucial factors in managing chronic conditions effectively
The benefits of data-driven gaps in care strategies
Implementing data-driven strategies to combat chronic conditions offers numerous benefits, including:
Improved patient outcomes
Early intervention and personalized care enable better health outcomes.
Reduced costs
Proactive management of chronic conditions can significantly reduce healthcare costs associated with complications and hospitalizations.
Enhanced patient engagement
Targeted outreach fosters better patient engagement and satisfaction.
Operational efficiency
Data-driven approaches optimize resource allocation and improve overall healthcare delivery efficiency.
Leveraging data for targeted interventions in chronic care management is not just a technological advancement—it's a paradigm shift in how we approach healthcare. By harnessing the power of data, you can offer more personalized, proactive and effective care, ultimately leading to better patient outcomes and a more efficient healthcare system.
9 effective gaps in care strategies
To effectively close gaps in care, healthcare organizations and payers should adopt a proactive, year-round clinical approach to improve patient outcomes and reduce long-term costs. Implementing programs throughout the year produces better results than late year-end pushes.
Here are nine effective gaps in care strategies you can employ any time.
1. Offer flexible testing options
Make it easy for patients to get screened by providing at-home testing kits for certain screenings. However, you must ensure the test quality meets reference lab standards and simplify the process for test completion and return. Flexible options remove barriers and increase participation rates.
2. Personalize patient engagement
Meet patients where they are by using multiple communication channels such as email, letters and text messages. Allow patients to choose their preferred communication method and implement reminder systems to boost response rates. Personalization can significantly improve patient engagement and compliance.
3. Collaborate with others in the healthcare community
Collaboration is key to successful gap closure. Payers, providers and others in the healthcare ecosystem can work together to identify target populations and specific care gaps. This includes sharing data and analytics to track progress and refine strategies, as well as collaborations ensuring comprehensive care throughout the year. You can also co-brand materials to increase patient trust and engagement.
4. Address barriers to care
To foster greater health equity, remove obstacles preventing patients from getting care. This includes targeting hard-to-reach geographical areas and offering support for patients with mobility or transportation challenges. Provide clear, accessible information about recommended screenings to educate and motivate patients.
5. Leverage data-driven insights
Let the numbers guide your strategy. Implement real-time analytics to track progress and use reporting tools to identify areas for improvement. Regularly adjust your strategies based on performance metrics to ensure optimal results.
6. Provide comprehensive support
Be there for patients throughout their healthcare journey. Make customer care teams available to answer questions and ensure patients understand how to take the tests appropriately and interpret the results. Provide follow-up support for positive test results to guide them through next steps.
7. Focus on cost-effectiveness
Consider balancing quality care with financial responsibility by developing opt-in programs instead of auto-deploy ones to manage costs. You can tailor your programs to meet specific organizational needs and goals while demonstrating the value of preventative care in reducing long-term healthcare costs to stakeholders.
8. Emphasize the human element
Remember patients are people first. Show them they’re cared for beyond just being part of a process. Offer a compassionate approach to potentially scary health screenings. This human touch can make a significant difference in compliance and satisfaction.
9. Continuously evaluate and improve
Conduct regular satisfaction surveys to gather patient feedback so the next program is constantly striving for better results. Analyze metrics to identify successes and areas for improvement. Then, build on successful initiatives to enhance future programs and continuously refine your approach. Implement systems for ongoing monitoring of patient data to identify care gaps in real time and establish a cadence of regular patient check-ins, either through telehealth or in-person visits.
When implementing these strategies, the key is to remain flexible, patient-centered and data-driven in your approach. Regularly reassess and adjust your strategies to ensure you're meeting the evolving needs of your patients and achieving optimal healthcare outcomes.
Using data to target patients in underserved communities
Lab data can also help you support socially vulnerable populations to enable health equity planning and location-based interventions. Using spatial visualization techniques to map health data geographically pinpoints hotspots and clusters of diabetes and CKD at the community level, allowing for more targeted interventions.
By following best practices to cultivate healthier, thriving communities, you can break down barriers to healthcare access for underserved communities, including those residing in the rural United States.
How Labcorp uses its data for chronic care management
With Labcorp, you have access to robust data powered by 45 billion lab results to improve your ratings and the health of your most vulnerable populations. Our targeted programs, analytics and digital tools help jump-start your gaps in care programs and enhance your chronic care management for patients with diabetes, CKD and hyperlipidemia.
Labcorp Insight Analytics® reports help you:
- Identify high-risk patients including those with co-morbidities and/or worsening conditions
- Target patients with overdue testing
- Generate actionable lists for care coordination teams to proactively engage patients and address health concerns
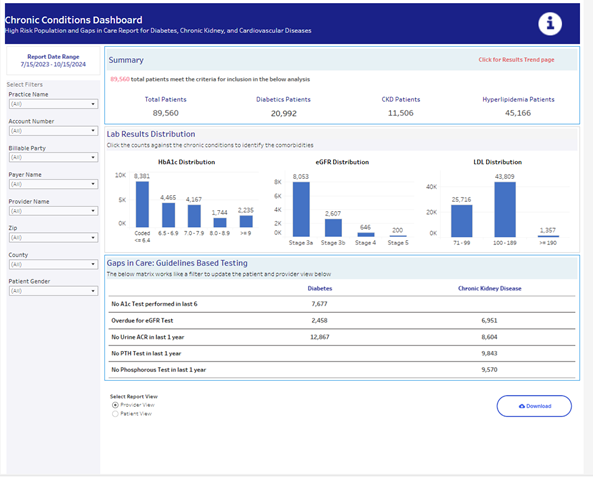
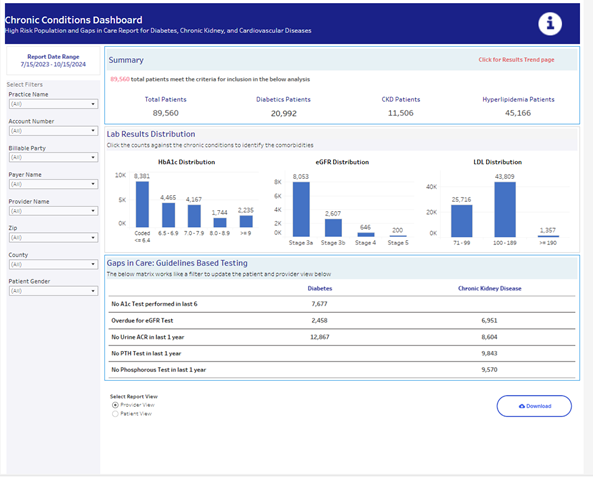
Insight Analytics offers interactive bar graphs for A1c, eGFR and LDL levels, allowing you to filter at-and rising-risk patients based on their latest test results. You also get guidelines-based care gaps for patients diagnosed with diabetes or CKD to ensure those patients get the appropriate testing based on their individual needs.
Contact us today to see how we can assist you in building effective targeted outreach programs for chronic disease.

